Data-Driven Enterprise Clinical Decision Support Solutions

Executive Summary
As the U.S. healthcare system approaches a $5 trillion spending threshold, the industry is shifting from infrastructure-heavy, reactive models toward digital-first, proactive care. Central to this transformation is the evolution of Clinical Decision Support (CDS) solutions from simple alerts to enterprise-wide Decision Intelligence. Currently, healthcare generates nearly 30% of the world’s data, yet the majority remains "dark" stored but unutilized for active clinical improvement. Furthermore, 76% of data leaders admit that organizational governance has not kept pace with AI adoption, creating a "governance lag" that threatens patient safety and data integrity.
This white paper provides a comprehensive roadmap for healthcare executives to implement scalable, data-driven CDS frameworks using the Pyramid Analytics Decision Intelligence Platform. By integrating data preparation, business analytics, and data science into a single, frictionless environment, organizations can bypass the traditional bottleneck of data duplication. This roadmap prioritizes direct query performance, no-code AI augmentation, and automated "Smart Insights" to empower everyone from the C-suite to the frontline. By following this strategic path, health systems can reduce administrative burnout, mitigate algorithmic bias, and ultimately transition from managing chronic disease to predicting and preventing it.
1. Introduction
Modern Healthcare CDS Landscape: From Reactive to Predictive)
The healthcare industry in 2026 is defined by a collision of unsustainable economic trajectories and exponential technological breakthroughs. With an aging population where one in five Americans will soon be over 65 demand for complex chronic care is surging, while workforce shortages continue to compress operational margins. Digital transformation is no longer a strategic choice but a survival imperative. Technology is shifting from a tool that augments healthcare to one that becomes the system, enabling "super consumers" to demand personalized, data-rich care experiences. AI adoption has accelerated faster than any previous technology, moving from a niche "buzzword" to an essential baseline for clinical and operational workflows.
Industry Trends at a Glance:
- Cognitive Augmentation: AI is now augmenting human cognition, allowing clinicians to function as data-orchestrators rather than just administrators.
- Virtual-First Delivery: Precision virtual infrastructure is eliminating geographical barriers, allowing for high-quality care at home.
- The $1 Trillion Shift: Reallocation of funds from outdated administrative overhead to AI-enabled intake and predictive care models
- Standardization of Care: Move toward "standard operating chassis" to reduce operational variability across hospital units.
2. Health Systems Enterprise CDS Challenges
Despite the abundance of healthcare data, enterprises face a paralyzing paradox: clinicians are drowning in paperwork while being starved for actionable insights. Physicians currently spend more than one-third of their time approximately 1.5 days a week on administrative rote, a leading cause of burnout and "pajama time" charting. Data siloing remains a primary antagonist; hospitals, labs, and wearables often maintain isolated records, making accountability for quality of care nearly impossible to track at scale.
Furthermore, an estimated 80% of clinical data is unstructured, creating "dark data" pools that traditional Business Intelligence (BI) tools fail to process effectively. Without a unified approach, AI pilots often fail to move into production because they lack a reliable data foundation or fail to integrate into human workflows.
Key Challenges:
- Fragmented Interoperability: Only 8% of primary care physicians find it "very easy" to use data from different EHR developers.
- Governance Lag: 56% of medical groups lack formal policies on AI use, leading to "Shadow AI" where staff use unapproved, risky consumer tools.
- Data Reliability: 57% of leaders view data quality as the top barrier to scaling AI from pilot to enterprise-wide impact.
- Inequitable Access: The "innovation divide" threatens to leave rural and underserved populations behind if equity is not built into CDS platforms from the start.
The healthcare sector is currently navigating a debilitating "trust paradox" that undermines the scalability of enterprise Clinical Decision Support (CDS) frameworks. While 65% of data leaders believe their internal workforces trust the data utilized for AI, approximately 76% admit that formal organizational governance has failed to keep pace with rapid technological adoption. This "governance lag" exposes organizations to significant vulnerabilities regarding privacy, security, and regulatory compliance. Furthermore, 81% of physicians express dissatisfaction with their employer's current speed of AI integration, often resorting to unauthorized "Shadow AI" tools that bypass established safety guardrails. These systemic vulnerabilities are compounded by complex contractual use limitations, where non-standardized NDAs and engagement letters often restrict the ability to feed high-quality patient context into generative models.
This administrative gridlock is deeply rooted in the "dark data" bottleneck, where the majority of healthcare’s information nearly 30% of the world's total volume is stored in unstructured clinical notes and isolated legacy databases. This fragmentation forces clinicians to spend more than one-third of their time on paperwork, directly fueling the 44% rate of physician burnout. To bridge this gap, enterprises must transition toward a "virtual by design" operating chassis that eliminates data siloing. By adopting unified platforms like Pyramid Analytics, which provide multi-source direct access to information without the friction of data duplication, organizations can transform their workforce from administrative clerks into data-orchestrators. This shift allows for the reallocation of annual spending from outdated overhead to AI-enabled, proactive care models.
3. The Architecture of Decision Intelligence for CDS
To overcome these challenges, health systems must pivot to Decision Intelligence, a unified approach that collapses the walls between data science, preparation, and business analytics. Unlike traditional BI, which often requires slow, costly data replication and complex coding, modern platforms prioritize direct access and no-code scalability. The goal is to provide a "single source of truth" where clinical and financial data are reconciled in real-time, allowing for immediate intervention. This architecture enables the creation of a "virtual semantic layer," which future-proofs analytical assets by allowing them to adapt as underlying data sources change.
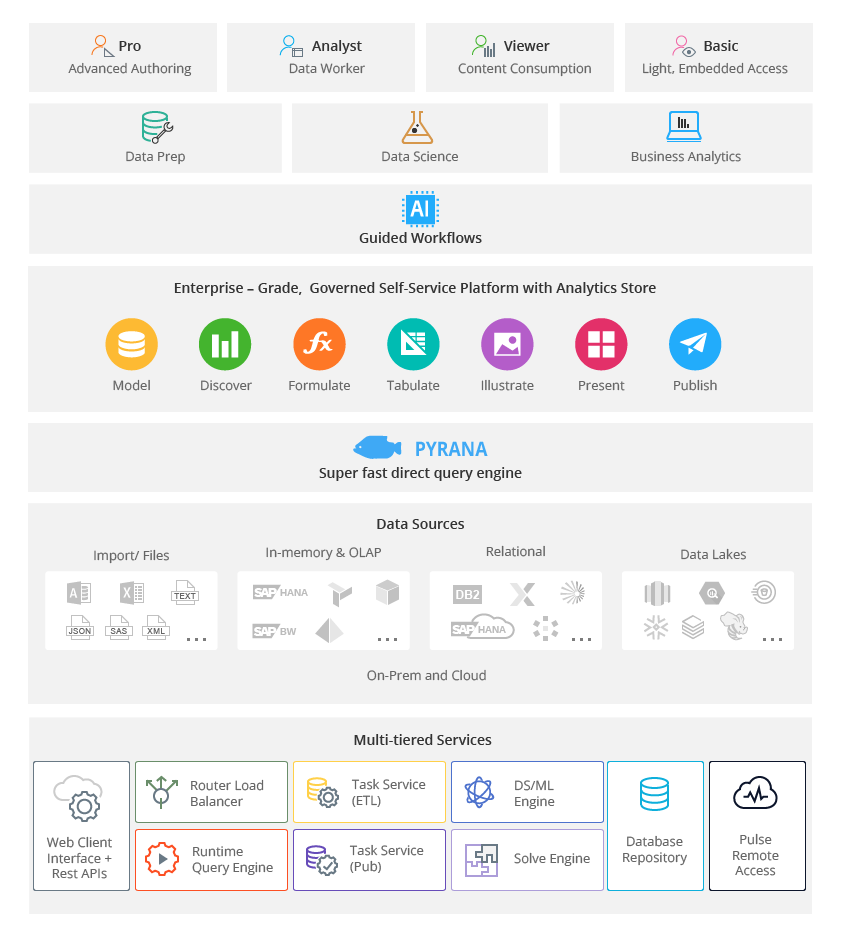
Figure 1 - PYRANA Direct Query Engine Informational Architecture (Source: Pyramid Analytics, 2025)
Pyramid Analytics Product Alignment:
"PYRANA" Direct Query Engine: Delivers 10x faster performance than traditional tools by querying data in-place across disparate sources (EHR, RCM, Labs) without duplication.
Generative BI & NLQ: A conversational interface leveraging Large Language Models (LLMs) allows non-technical staff to ask complex questions like, "What is our current sepsis readmission trend?" and receive instant visualizations.
AI-Automated "Smart Insights": Automatically identifies the root causes of anomalies or care gaps, identifying key drivers and influencers without manual analysis.
Enterprise Governance: Provides the "robust control" needed to manage row-level security and data lineage, ensuring CDS outputs are both trusted and auditable.
4. Key Pillars of an Enterprise CDS Roadmap
A successful enterprise CDS implementation requires a multi-layered strategic roadmap that prioritizes immediate clinician relief and long-term predictive capability. This roadmap begins with acceptance and adoption, ensuring that tools are perceived as useful and easy to use by frontline caregivers. Organizations must then transition to building a "standard operating chassis" that unifies disparate data services into a single, cohesive platform. By anchoring the strategy in the clinician experience, leadership can measure success not just by efficiency gains, but by the "capacity to care"restoring time for the patient-physician relationship.
Strategic Action Steps:
- Unshackle "Dark Data": Use multi-source direct access to query trapped clinical information without the lag of data movement.
- Redesign Workflows: Fundamentally change how tasks like documentation and triage are handled, rather than simply layering technology over old processes.
- Deploy Real-Time Predictive Alerts: Integrate models like the Epic Sepsis Model or readmission risk predictors directly into the clinical workflow.
- Scale Through Self-Service: Empower business analysts and clinical leaders to build their own dashboards using no-code tools, reducing the IT backlog.
5. AI Governance: Ensuring Ethics and Trust in Automated Decisions
As AI becomes integral to clinical decision-making, the risks of "confabulations" (hallucinations) and algorithmic bias must be managed through rigorous oversight. Governance is no longer just about compliance; it is the cornerstone of trust in the healthcare ecosystem. Medical groups must establish "human-in-the-loop" frameworks where clinicians remain the final decision-makers, supported by AI that is transparent and explainable. Furthermore, emerging regulations like the 2025 HIPAA Security Rule updates mandate that AI tools be included in formal risk assessments and security audits.
The FAVES Principles for CDS Governance:
Fair: Does the algorithm perform consistently across different patient demographics?
Appropriate: Is the AI being used for a clinical task that requires human judgment?
Valid/Effective: Is there real-world evidence that the tool works in this specific specialty?
Safe: Are there clear failure modes and "buried point layers" to catch errors quickly?
Risk Mitigation Strategy:
- Standardize Data Mapping: Use ML-driven harmonization to ensure disparate lab codes (LOINC) and diagnosis descriptions (ICD) are consistent.
- Audit "Shadow AI": Identify unauthorized consumer tool use and provide safe, enterprise-approved paths.
6. Implementation Strategy: Moving from Pilot to Scaled Impact
The transition from isolated experiments to enterprise-level value represents the "breaking point" for most health systems. High-performing organizations differentiate themselves by thinking beyond incremental efficiency to transformative innovation. This requires a dual-speed approach: building resilience through immediate operational improvements while simultaneously redesigning for a "virtual by design" future. Successful scale depends on workforce upskilling, as 75% of data leaders note that employees require enhanced data literacy to responsibly use AI in daily operations.
Execution Framework:
Establish a Governance Committee: Multi-disciplinary teams including clinicians, IT security, and legal counsel must oversee the AI lifecycle.
Utilize a "Push System" for Reporting: Shift from one-off data requests to automated, periodic metric reviews that inform strategic decisions.
Invest in Infrastructure: Spend time building a solid foundation of data stacks and LLMs before scaling across the organization.
Case Study Achievement: By adopting Pyramid Analytics, The Physician Alliance saved $350,000 annually and democratized trapped data for 2,400 physicians, demonstrating the ROI of unified Decision Intelligence.
7. Conclusion
Healthcare stands at a definitive inflection point. The traditional, infrastructure-heavy model is collapsing under the weight of rising costs and administrative complexity, replaced by a distributed, tech-enabled system. For enterprise leaders, the path forward requires moving beyond the role of administrator to becoming a data-orchestrator who prioritizes clinical judgment over paperwork. Success in this new era will not be defined by who has the most sophisticated algorithm, but by who builds the most trusted, integrated, and governed ecosystem for decision-making.
The Pyramid Analytics Decision Intelligence Platform serves as the critical operating chassis for this journey, providing the speed, flexibility, and governance required to turn vast amounts of clinical data into actionable insights. By implementing the roadmap outlined in this paper focusing on direct data access, clinical-first AI, and robust governance enterprises can bridge the innovation divide and ensure financial resilience. The $1 trillion shift is coming; those who lead with Decision Intelligence will not only survive the transformation but will redefine the standard of care for the next generation.
8. References
- American Medical Association. (2025). Practice ownership linked to physicians’ use of telehealth.
- Brooks Pierce. (2026). The Need for Comprehensive Governance of AI Use in Health Care Settings.
- Cigna Healthcare. (2026). The top health care trends for 2026.
- Elation Health. (2026). Predictions for Primary Care in 2026.
- Informatica. (2026). CDO Insights 2026: Data governance and the trust paradox.
- IntuitionLabs. (2026). Impact of AI on Clinical Data Management in the US.
- JAMA Network. (2024). Primary Care Physicians’ Satisfaction With Interoperable HIT.
- McKinsey & Company. (2025). The State of AI: Global Survey 2025.
- McKinsey & Company. (2026). McKinsey perspectives on healthcare industry trends.
- MGMA. (2026). AI governance in medical group practices.
- Oracle. (2025). Oracle AI Database 26ai.
- Praxis EMR. (2026). Physicians choose their top 10 EHR systems for 2026.
- PwC. (2025). From breaking point to breakthrough: the $1 trillion opportunity.
- Pyramid Analytics. (2026). The Physician Alliance - Case Study.
- Society of General Internal Medicine. (2024). Recommendations on the Use of Generative AI in Medicine.
 Request a meeting
Request a meeting
 Email
Email Call
Call EN
EN
 FR
FR
 ES
ES

















Add Comments